POCUS – EMERGENCY ULTRASOUND
There are various names to describe these procedures. They involve scans of the abdomen, thorax and heart to give rapid information about a critical patient in a non-invasive low stress manor.
· POCUS – Point of Care Ultrasound Scan
- A general term that includes cardiac, thoracic and abdominal scans
· AFAST & TFAST – Abdominal & Thoracic Focused Assessment with Sonography for Trauma, Triage and Tracking
· Focused cardiac ultrasonography (FCU)
POCUS BASIC USE
- As a quick screen for potentially life-threatening problems:
1. Is there an abdominal effusion?
- The scan can identify the effusion, narrow down differentials, and locate appropriate windows for abdominocentesis
2. Is there free fluid in the pleural space?
- Provide oxygen and performs a thoracocentesis asap
- (Unless a coagulopathy related haemothorax is suspected in which case assess clotting first, e.g. rat bait cases)
3. Is there a pericardial effusion?
- If the patient is unstable this needs draining asap
4. Is there interstitial or alveolar fluid? (wet lung)
- If so, is the left atrium enlarged which could make cardiac causes more likely?
- If the assessment of the left atrium is not possible this judgement can be made via the clinical exam
o Heart murmur, arrythmia, pulmonary crackles etc. may increase the suspicion of left sided congestive heart failure as can the response to frusemide (radiographs to confirm when more stable)
o An abnormal Pro BNP blood test can also help the clinician suspect a cardiac cause of dyspnoea over a respiratory cause if ultrasound is unavailable
5. Is there a pneumothorax or consolidated lung?
COMMON INDICATIONS FOR A POCUS
· Collapsed/Critical patients:
- Screen for free fluid in the abdominal, pleural and pericardial space. Free fluid can be found in almost three quarters of unstable critical cases
- Facilitate guided abdo/thoracocentesis where appropriate for treatment & diagnostics
· Trauma patients:
- Free fluid screening – haemoabdomen, uroperitoneum. Track changes over time
- Pneumothorax (lack of glide sign) etc.
· Dyspnoea:
- Identification of pleural effusions
A very common cause of dyspnoeic cats
Can help to narrow down differentials
- Identify alveolar or interstitial fluid “wet lung”
Common ddx pulmonary oedema, pneumonia, neoplasia etc
- Confirm suspected L-CHF
Wet lung plus enlarged LA
- Identify consolidated lung – pneumonia, neoplasia
- Pneumothorax
Lack of glide sign
Altered M-mode
Note – Radiography is a superior modality of assessing the lungs but is often not safe to do initially in dyspnoeic patients. POCUS can give you useful information in the meantime to help guide diagnostics and treatment
Coagulopathy cases:
- Screen for free fluid - haemothorax/abdomen
Acute abdomen cases
Post-surgical unstable patients:
- Free fluid which could indicate bleeding or peritonitis etc.
Certain anaemic patients:
- Identify internal bleeding, obvious masses, organomegaly etc.
Urethral obstruction/urinary cases:
- Screen for uroperitoneum etc.
HOW TO DO A POCUS
Stabilise where appropriate first:
- Oxygen
- IV line and fluids
- Thoracocentesis - can be performed blind if there is a high suspicion of pneumothorax/pleural effusion from the exam
Patient prep:
May need to clip vs alcohol +/- gel and part the hair only.
Positioning:
Sternal/standing for any dyspnoeic patient.
Otherwise, lateral recumbency could be used.
1. Left and right chest tube sites
o Approx 7th to 9th intercostal spaces
o Place the probe on perpendicular to the chest wall
o For pulmonary parenchymal disease, oedema etc.
o Pneumothorax assessment
2. Left and right pericardial sites
o Approx 5th – 6th intercostal space
o Pericardial effusion assessment
o Pleural fluid assessment
o Basic assessment of left atrial size on the right
3. Diaphragmatic-hepatic window
o Place probe at the xiphoid and point cranially. Zoom out to image heart, pericardium and pleural space for fluid
NORMAL VS ABNORMAL PATHOLOGY
1. Left and right chest tube sites
“Normal view” – A-lines and glide sign:
A-LINES – Horizontal lines – pleural line reverberation artefact
· Seen with normal lung parenchyma if there is a normal “glide sign”
- The glide sign is the normal motion of the pleural line back and forth as the patient breathes
· If there are A-lines but no glide sign, the patient could have a pneumothorax
- Test thoracocentesis to confirm and treat
- There are M-mode assessments that can be performed to aid in pneumothorax identification but are beyond the scope of this introduction to POCUS section
B-LINES – Vertical lines (“Rocket-lines”/” Wet-lung”)
- Vertical hyperechoic lines
- Indicate interstitial-alveolar pulmonary pathology. Ddx:
o Pulmonary oedema
o Non-cardiogenic pulmonary oedema – Includes haemorrhage, neoplasia, acute respiratory distress syndrome (ARDS) etc.
o Pneumonia
o Contusion etc.
- Occasional B-lines are normal
- 3 or more B- lines at one site is abnormal
Above cine loop - Normal A lines and glide sign
Above cine loop - Multiple B-lines
CONSOLIDATED LUNG
· Fluid or cells infiltrating the lung from pneumonia, pulmonary neoplasia, lung contusion or torsion
· Instead of normal A-lines - Hyperechoic foci with distal shadowing in early mild cases to “hepatised lung” in more advanced severe cases where the lung appears similar to the liver – Air filled bronchi show as hyperechoic air filled bronchograms and small hyperechoic foci represent air in the alveoli
· The lung retains its normal volume and shape unlike in atelectasis where the lung volume is reduced – often due to pressure from a PLE for example
1. Left and right pericardial sites
- Basic assessment of heart on the right
o Is the left atrium enlarged?
o Is the heart enlarged in general?
o Is the contractility subjectively reduced?
- Pericardial effusion assessment
- Pleural fluid assessment
Basic heart assessment (focused cardiac ultrasound)
The right parasternal long axis view can be used for a subjective assessment of left atrial size too. B-lines plus an enlarged LA would be suggestive of pulmonary oedema secondary to CHF e.g. from MVD.
Above images depict two still images of the right parasternal 4 chamber view of the heart. This is a good initial view to subjectively assess chamber size and contractility. The left image is of a dog with no clinical signs in early stage B1 MVD. Note the normal bullet shaped left ventricle (LV) and the angular square-ish left atrium (LA). On the right is a dog with advanced MVD going into CHF. Note the abnormally large and rounded LV and LA. They are volume overloaded. The thickened irregular mitral valve can also be seen.
Right parasternal 4 chamber view of a dog with B1 MVD. The chamber sizes are normal
POCUS right parasternal 4 chamber view of a dog with severe MVD and left atrial enlargement
POCUS in a cat with HCM but a normal La size. Right parasternal 4 chamber view
La Max in this cat is normal at 13.4mm (16mm and above is abnormal)
If this cat was dypsnoeic a cardiac cause would be unlikely
La Max in this cat is >20mm. The dyspnoea is likely to be cardiac related
Right parasternal 4 chamber view in a cat with an end-stage cardiomyopathy. Comparing to the other cine loop we can see a much larger La with poorer contractility
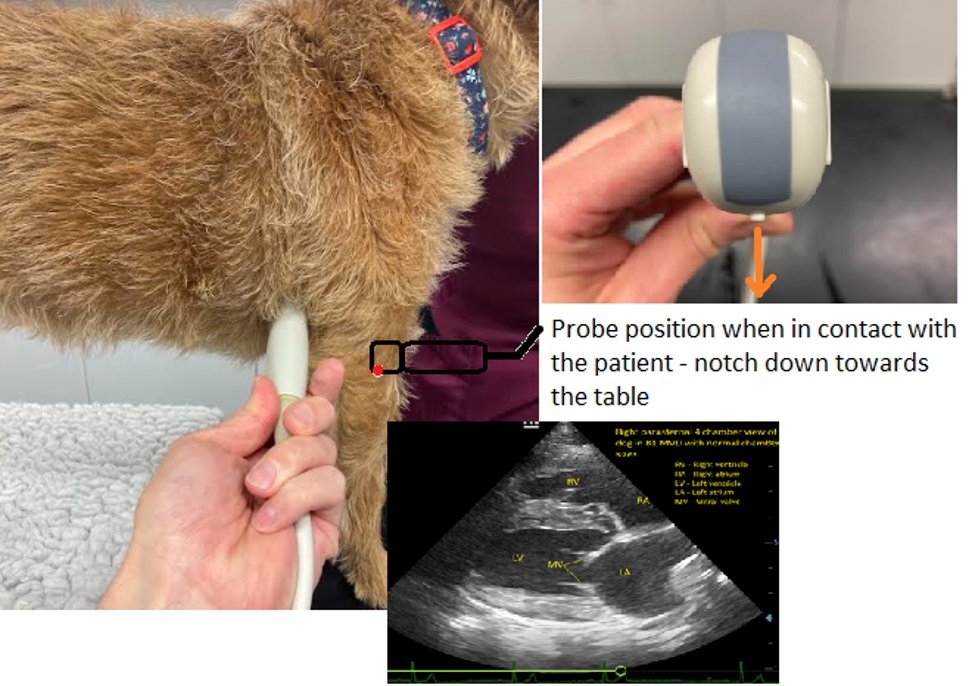
Obtaining the right parasternal 4 chamber view:
· Select probe and cardiac settings if available. Whilst a phased array probe is best for echocardiography a microconvex probe will work fine for POCUS
· Be aware of the probe orientation marker. This will help to orient you during scanning. For scanning the author prefers to have this marker on the left of the screen (see below image)
With the patient standing or in sternal (preferable over recumbency for the dyspnoeic/stressed patient), feel for the apex beat of the heart in the right axilla.
Place the probe on the chest in this location in the intercostal space, marker down towards the table/nearest the sternum
· Keep the probe perpendicular to the chest wall for this view
· Make very slight probe adjustments to achieve the 4 chamber view
· If the image is tilted, moving slightly up the chest wall away from the sternum can make the image more horizontal
Short axis left atrium to aorta view
This view can be used to quantitatively assess the size of the left atrium by comparing the size of the aorta to that of the left atrium.
· In dogs and cats a LA/Ao ratio >1.5 is abnormal but of course heart enlargement can occur before CHF develops (stage B2 MVD)
· A LA/Ao >2.0 in a dog or a cat with compatible clinical signs and B-lines is highly suggestive of L-CHF
· A LA/Ao <1.6 + normal A-lines = no L-CHF
· A normal LA/Ao <1.6 + B-lines is more likely to be related to pneumonia or non cardiogenic oedema (haemorrhage, neoplasia, ARDS etc.)
The left image shows a dog with a normal LA/Ao ratio – there is no left atrium enlargement in this patient meaning any B-lines present in this patient are less likely to be related to L-CHF.
The right image shows an abnormal LA/Ao ratio of 2.42. This patient has dyspnoea and B-lines on the chest. The cause is very likely to be L-CHF.
Above cine loops of the La/Ao short axis view. One with a normal ratio and the other in a dog abnormal - it has severe La enlargement secondary to mitral dysplasia
Obtaining the La/Ao short axis view:
· Start by obtaining the right parasternal 4 chamber image as above with the probe indicator pointing down towards the table. Ensure the image is horizontal on the screen
· Whilst keeping the probe in the same place, rotate it 90 degrees clockwise until the notch is pointing caudally towards the patients bottom. This will bring in the mushroom view (right parasternal short axis view at the level of the papillary muscles)
Above image shows the right parasternal short axis view of the heart at the level of the papillary muscles. Aka the mushroom view. The hyperechoic bright line at the bottom represents the pericardium. This view is useful to screen for pericardial effusions and can give a gross indication of contractility
Dog with DCM. Note the poor contractility and dilated left ventricle compared to the normal cine loop mushroom view before
To obtain the La/Ao short axis view from the mushroom:
· Fan cranially towards the head (drop the tail of the probe) to fan through different levels of the short axis view
· Mushroom - fish mouth view of the mitral valve - La/Ao
Above cine loop in a dog with DCM showing the views in sequence. Start of the loop shows the right parasternal 4 chamber view. Rotating the probe “thumb to bum” brings in the 5 chamber and then mushroom view. Dropping the tail of the probe and fanning towards the head brings in the mushroom view and then La/Ao
PLEURAL EFFUSIONS
Pleural effusions can be picked up at the pericardial sites/caudoventral thorax
The above image shows a pleural effusion in a cat with heart failure (black anechoic fluid). Fibrin strands can be seen floating in this fluid.
Pleural effusion differentials:
· Cardiac – right sided congestive heart failure, pericardial effusion, cardiomyopathy secondary to hypertrophic cardiomyopathy or hyperthyroidism in cats
· Neoplasia
· Haemothorax – trauma, coagulopathy
· Pyothorax
· Pleuropneumonia
· Diaphragmatic hernia
· Hypoproteinaemia
· FIP
Oxygen should be provided and urgent thoracocentesis should be performed. Post drain radiographs screen for causes such as pulmonary masses. The POCUS (or a pro-BNP if ultrasound is unavailable) may help identify a cardiac cause. Fluid analysis and bloodwork including T4 (cats) should also be performed. See the dyspnoeic cat and pleural effusions section
PERICARDIAL EFFUSIONS
The above image shows a pericardial effusion (PE) between the heart and the pericardium. The right image shows evidence of tamponade. The right atrium (RA) is collapsing under the pressure of the pericardial fluid (red arrow). This reduces cardiac output leading to weakness and collapse. Emergency pericardiocentesis is required.
The above image shows a pericardial effusion in a dog with neoplasia, likely haemangiosarcoma.
Occasionally it can be tricky to differentiate pleural effusion from pericardial effusion. The trick is to identify the fluid sitting between the LV and white line representing the pericardium. It can be helpful to look at different views as in the above image, to help confirm the PE. The diaphragmatic hepatic view can also be a useful view for diagnosing PE’s around the apex of the heart (see the section below)
Pericardial effusion ddx:
· Neoplasia and idiopathic predominantly
· Severe MVD with LA rupture
· Coagulopathy
· Trauma
If the patient is stable (no collapse, dyspnoea, tachycardia etc.), without tamponade, detailed echocardiography should be performed to screen for cardiac neoplasia. The right atrium and in particular the right auricle should be scrutinised. This likely requires referral. Unstable patients need to be drained asap. See pericardial effusion section
1. Diaphragmatic-hepatic (DH) window
Can look through the liver into the thorax to screen for:
· Pleural fluid
· Pericardial effusion
Place the probe just caudal to the xiphoid process and look cranially. Often need to zoom out to bring the heart in through the diaphragm and it can take some probe pressure to get the view
Above image and cine loop show a normal DH view
Above image shows a DH view in a patient with a pericardial effusion. This has led to ascites developing due to R-CHF.
ABDOMINAL EMERGENCY ULTRASOUND (AFAST)
1. Diaphragmatic hepatic view
2. Cystocolic window
3. Splenorenal window
4. Hepatorenal window
5. Umbilical/dependent view
1. Diaphragmatic hepatic view
o As per the T-Fast view
o Place the probe at the xiphoid and scan cranially. Zoom out to image heart, pericardium and pleural space for fluid. Fan the probe to see if there is free fluid between liver lobes, check gall bladder etc.
Above image - Note the black, hypoechoic fluid between the liver lobes. The liver itself is heterogenous and contains hypoechoic nodules. The edges of the liver are irregular. This is often seen in end-stage cirrhosis in dogs.
Above cine loop DH view - Note the ascites between the diaphragm and the liver and pleural effusion. 15 year old cat with a cardiomyopathy and heart failure
2. Cystocolic window
o Assess the bladder and screen for caudal peritoneal effusions
Normal cystocolic view in a dog
Note the area highlighted by the yellow circle in the above image. It appears to show a hole in the bladder wall. This is actually just a refraction artefact commonly seen when there is an abdominal effusion. It is not indicative of bladder rupture.
If concerned about a uroabdomen obtain a sample of the free fluid via abdominocentesis. Run this through the biochemistry machine testing for creatinine. Compare this to the serum creatine. An abdominal fluid creatine to serum creatine ratio >2 to 1 has a 100% specificity and 86% sensitivity for uroabdomen.
3. Splenorenal window
o Position on left kidney then fan cranio-laterally to include the spleen
o Screen for free fluid, splenic masses etc.
4. Hepatorenal window
o Image from underneath when in R recumbency or via the right side in larger dogs
o Find right kidney and fan cranially to include the liver
o Screen for free fluid etc.
5. Umbilical/dependent view
o This is normally the most gravity dependent part of the abdomen where fluid often accumulates in a standing patient
Above cine loop - Mild peritoneal effusion in a dog with a protein losing enteropathy
Above cine loop - Large effusion in a dog secondary to a pericardial effusion
Ascites differentials:
· Haemoabdomen
- Trauma
- Neoplasia (commonly a ruptured splenic mass)
- Coagulopathy
- Note – The PCV of the abdominal fluid in haemoabdomen cases should be similar to the peripheral blood in active bleeding
· Transudate
- Hypoproteinaemia (Protein losing nephropathy, Protein losing enteropathy, Liver failure)
Check blood albumin levels
Check a urine protein creatine ratio to screen for PLN
A bile acid stimulation test can help screen for liver failure
- Portal hypertension
· Modified transudate – Cardiac (R-CHF), pericardial effusion, hepatic disease, neoplasia, pancreatitis, chronic transudates
· Exudate – Septic, FIP, bile peritonitis, uroabdomen, pancreatitis
· Chyle – Obstructed lymph system – cardiac, neoplasia, inflam etc.